Vasculitis
| Vasculitis | |
|---|---|
| Other names | Vasculitides[1] |
 | |
| Petechia and purpura on the lower limb due to infection-associated vasculitis. | |
| Pronunciation | |
| Specialty | Rheumatology, Immunology |
| Symptoms | Weight loss, fever, myalgia, purpura, abdominal pain |
| Complications | Gangrene, Myocardial infarction |
Vasculitis is a group of disorders that destroy blood vessels by inflammation.[2] Both arteries and veins are affected. Lymphangitis (inflammation of lymphatic vessels) is sometimes considered a type of vasculitis.[3] Vasculitis is primarily caused by leukocyte migration and resultant damage. Although both occur in vasculitis, inflammation of veins (phlebitis) or arteries (arteritis) on their own are separate entities.
Signs and symptoms
[edit]The clinical presentation of the various vasculitides on the skin and internal organs is mostly determined by the diameter or size of the vessels mainly affected.[4] Non-specific symptoms are common and include fever, headache, fatigue, myalgia, weight loss, and arthralgia.[5][6]
All forms of vasculitis, even large vessel vasculitides, may cause skin manifestations. The most common skin manifestations include purpura, nodules, livedo reticularis, skin ulcers, and purpuric urticaria.[7]
| Type | Name | Main symptoms |
|---|---|---|
| Primary large vessel vasculitis[8] | Takayasu arteritis | Diminished or absent pulses, vascular bruits, hypertension, Takayasu retinopathy, and aortic regurgitation.[9] |
| Giant cell arteritis | Headache, scalp tenderness, jaw claudication, and blindness.[10] | |
| Primary medium vessel vasculitis[8] | Polyarteritis nodosa | Mononeuritis multiplex, nodules, purpura, livedo, and hypertension.[11] |
| Kawasaki disease | Fever, conjunctivitis, exanthema, palmoplantar erythema, cervical lymphadenopathy, and mucosal enanthema.[12][13] | |
| Primary small vessel antineutrophil cytoplasmic antibody (ANCA)–associated vasculitis[8] | Microscopic polyangiitis | Focal segmental rapidly progressive glomerulonephritis, proteinuria, hemoptysis, palpable purpura, abdominal pain, and peripheral neuropathy.[14] |
| Granulomatosis with polyangiitis | Crusting rhinorrhea, sinusitis, chronic otitis media, nasal obstruction, shortness of breath, and chronic cough. [15] [16] | |
| Eosinophilic granulomatosis with polyangiitis | Asthma, allergic rhinitis, sinusitis, nasal polyps, peripheral neuropathy, pulmonary infiltrates, and abdominal pain.[17][18] | |
| Primary immune complex small vessel vasculitis[8] | Anti-glomerular basement membrane disease | Glomerulonephritis, lung hemorrhage, hematuria, hemoptysis, cough, and dyspnea.[19] |
| Cryoglobulinemic vasculitis | Palpable purpura, Raynaud's phenomenon, joint pain, and peripheral neuropathy.[20] | |
| IgA vasculitis | Palpable purpura, arthralgia, abdominal pain, nephritis, and haematuria.[21] | |
| Hypocomplementemic urticarial vasculitis | Hives, arthralgia, membranoproliferative glomerulonephritis, and chronic obstructive pulmonary disease.[22] | |
| Primary variable vessel vasculitis[8] | Behcet’s disease | Oral ulcers, genital ulcers, papulopustular lesions, uveitis, superficial venous thrombosis and deep vein thrombosis.[23] |
| Cogan’s syndrome | Interstitial keratitis, ocular redness, vertigo, and tinnitus.[24] | |
| Single-organ vasculitis[25][8] | Cutaneous small-vessel vasculitis | Palpable purpura, necrosis, ulceration, bullae, and nodules.[26] |
| Cutaneous arteritis | Nodules, livedo reticularis, ulcers, and gangrene.[27] | |
| Primary central nervous system vasculitis | Headache, cognitive impairment, stroke, encephalopathy, and seizures.[28] | |
| Retinal vasculitis | Visual impairments, floaters, and macular edema.[29] | |
| Secondary vasculitis[8] | Lupus vasculitis | Palpable purpura, petechiae, papulonodular lesions, urticaria lesions, and mononeuritis multiplex.[30] |
| Rheumatoid vasculitis | Purpura, focal digital lesions, ulcers, digital necrosis, pyoderma, distal sensory or motor neuropathy, and mononeuritis multiplex.[31] |
Causes
[edit]There are several different etiologies for vasculitides. Although infections usually involve vessels as a component of more extensive tissue damage, they can also directly or indirectly cause vasculitic syndromes through immune-mediated secondary events. Simple vascular thrombosis usually only affects the luminal process, but through the process of thrombus organization, it can also occasionally cause a more chronic vasculitic syndrome. The autoimmune etiologies, a particular family of diseases characterized by dysregulated immune responses that produce particular pathophysiologic signs and symptoms, are more prevalent.[32]
Classification
[edit]Primary systemic, secondary, and single-organ vasculitis are distinguished using the highest classification level in the 2012 Chapel Hill Consensus Conference nomenclature.[33]
Primary systemic vasculitis
[edit]Primary systemic vasculitis is categorized by the size of the vessels mainly involved. Primary systemic vasculitis includes large-vessel vasculitis, medium-vessel vasculitis, small-vessel vasculitis, and variable-vessel vasculitis.[33]
Large vessel vasculitis
[edit]The 2012 Chapel Hill Consensus Conference defines large vessel vasculitis (LVV) as a type of vasculitis that can affect any size artery, but it usually affects the aorta and its major branches more frequently than other vasculitides.[33] Takayasu arteritis (TA) and giant cell arteritis (GCA) are the two main forms of LVV.[8]
Medium vessel vasculitis
[edit]Medium vessel vasculitis (MVV) is a type of vasculitis that mostly affects the medium arteries, which are the major arteries that supply the viscera and their branches. Any size artery could be impacted, though.[33] The two primary types are polyarteritis nodosa (PAN) and Kawasaki disease (KD).[8]
Small vessel vasculitis
[edit]Small vessel vasculitis (SVV) is separated into immune complex SVV and antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis (AAV).[33]
Antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis (AAV) is a necrotizing vasculitis linked to MPO-ANCA or PR3-ANCA that primarily affects small vessels and has few or no immune deposits. AAV is further classified as eosinophilic granulomatosis with polyangiitis (EGPA), granulomatosis with polyangiitis (GPA), and microscopic polyangiitis (MPA).[33]
Immune complex small vessel vasculitis (SVV) is vasculitis that primarily affects small vessels and has moderate to significant immunoglobulin and complement component deposits on the vessel wall.[33] Normocomplementemic urticarial vasculitis (HUV) (anti-C1q vasculitis), cryoglobulinemic vasculitis (CV), IgA vasculitis (Henoch-Schönlein) (IgAV), and anti-glomerular basement membrane (anti-GBM) disease are the categories of immune complex SVV.[8]
Variable vessel vasculitis
[edit]Variable vessel vasculitis (VVV) is a kind of vasculitis that may impact vessels of all sizes (small, medium, and large) and any type (arteries, veins, and capillaries), with no particular type of vessel being predominantly affected.[33] This category includes Behcet's disease (BD) and Cogan's syndrome (CS).[8]
Secondary vasculitis
[edit]The subset of illnesses known as secondary vasculitis are those believed to be brought on by an underlying ailment or exposure. Systemic illnesses (such as rheumatoid arthritis), cancer, drug exposure, and infection are the primary causes of vasculitis; however, there are still few factors that have a conclusively shown pathogenic relationship to the condition.[34] Vasculitis frequently coexists with infections, and several infections, including hepatitis B and C, HIV, infective endocarditis, and tuberculosis, are significant secondary causes of vasculitis.[35] Except for rheumatoid vasculitis, the majority of secondary vasculitis forms are exceedingly rare.[36]
Single-organ vasculitis
[edit]Single-organ vasculitis, formerly known as "localized," "limited," "isolated," or "nonsystemic" vasculitis, refers to vasculitis that is limited to one organ or organ system. Examples of this type of vasculitis include gastrointestinal, cutaneous, and peripheral nerve vasculitis.[34]
Diagnosis
[edit]
- Laboratory tests of blood or body fluids are performed for patients with active vasculitis. Their results will generally show signs of inflammation in the body, such as increased erythrocyte sedimentation rate (ESR), elevated C-reactive protein (CRP), anemia, increased white blood cell count and eosinophilia. Other possible findings are elevated antineutrophil cytoplasmic antibody (ANCA) levels and hematuria.
- Other organ functional tests may be abnormal. Specific abnormalities depend on the degree of various organs involvement. A brain SPECT can show decreased blood flow to the brain and brain damage.
- The definite diagnosis of vasculitis is established after a biopsy of involved organ or tissue, such as skin, sinuses, lung, nerve, brain, and kidney. The biopsy elucidates the pattern of blood vessel inflammation.
- Some types of vasculitis display leukocytoclasis, which is vascular damage caused by nuclear debris from infiltrating neutrophils.[37] It typically presents as palpable purpura.[37] Conditions with leucocytoclasis mainly include hypersensitivity vasculitis (also called leukocytoclastic vasculitis) and cutaneous small-vessel vasculitis (also called cutaneous leukocytoclastic angiitis).
- An alternative to biopsy can be an angiogram (x-ray test of the blood vessels). It can demonstrate characteristic patterns of inflammation in affected blood vessels.
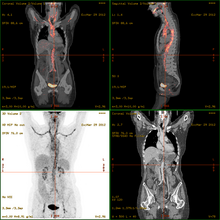
- 18F-fluorodeoxyglucose positron emission tomography/computed tomography (FDG-PET/CT)has become a widely used imaging tool in patients with suspected Large Vessel Vasculitis, due to the enhanced glucose metabolism of inflamed vessel walls.[38] The combined evaluation of the intensity and the extension of FDG vessel uptake at diagnosis can predict the clinical course of the disease, separating patients with favourable or complicated progress.[39]
- Acute onset of vasculitis-like symptoms in small children or babies may instead be the life-threatening purpura fulminans, usually associated with severe infection.
| Disease | Serologic test | Antigen | Associated laboratory features |
|---|---|---|---|
| Systemic lupus erythematosus | ANA including antibodies to dsDNA and ENA [including SM, Ro (SSA), La (SSB), and RNP] | Nuclear antigens | Leukopenia, thrombocytopenia, Coombs' test, complement activation: low serum concentrations of C3 and C4, positive immunofluorescence using Crithidia luciliae as substrate, antiphospholipid antibodies (i.e. anticardiolipin, lupus anticoagulant, false-positive VDRL) |
| Goodpasture's disease | Anti-glomerular basement membrane antibody | Epitope on noncollagen domain of type IV collagen | |
| Small vessel vasculitis | |||
| Microscopic polyangiitis | Perinuclear antineutrophil cytoplasmic antibody | Myeloperoxidase | Elevated CRP |
| Granulomatosis with polyangiitis | Cytoplasmic antineutrophil cytoplasmic antibody | Proteinase 3 (PR3) | Elevated CRP |
| Eosinophilic granulomatosis with polyangiitis | perinuclear antineutrophil cytoplasmic antibody in some cases | Myeloperoxidase | Elevated CRP and eosinophilia |
| IgA vasculitis (Henoch-Schönlein purpura) | None | ||
| Cryoglobulinemia | Cryoglobulins, rheumatoid factor, complement components, hepatitis C | ||
| Medium vessel vasculitis | |||
| Classical polyarteritis nodosa | None | Elevated CRP and eosinophilia | |
| Kawasaki's Disease | None | Elevated CRP and ESR |
In this table: ANA = antinuclear antibodies, CRP = C-reactive protein, ESR = erythrocyte sedimentation rate, dsDNA = double-stranded DNA, ENA = extractable nuclear antigens, RNP = ribonucleoproteins; VDRL = Venereal Disease Research Laboratory
Treatment
[edit]Treatments are generally directed toward stopping the inflammation and suppressing the immune system. Typically, corticosteroids such as prednisone are used. Additionally, other immune suppression medications, such as cyclophosphamide and others, are considered. In case of an infection, antimicrobial agents including cephalexin may be prescribed. Affected organs (such as the heart or lungs) may require specific medical treatment intended to improve their function during the active phase of the disease.[citation needed]
See also
[edit]References
[edit]- ^ "Vasculitis — Definition". Merriam-Webster Online Dictionary. Archived from the original on 1 July 2016. Retrieved 8 January 2009.
- ^ "Glossary of dermatopathological terms. DermNet NZ". Archived from the original on 20 December 2008. Retrieved 8 January 2009.
- ^ "Vasculitis" at Dorland's Medical Dictionary
- ^ Sunderkötter, Cord (2022). "Vasculitis and Vasculopathies". Braun-Falco´s Dermatology. Berlin, Heidelberg: Springer Berlin Heidelberg. pp. 1125–1169. doi:10.1007/978-3-662-63709-8_64. ISBN 978-3-662-63708-1.
- ^ Luqmani, Raashid; Robson, Joanna; Suppiah, Ravi (August 2018). "272: Vasculitis". In Davey, Patrick; Sprigings, David (eds.). Diagnosis and Treatment in Internal Medicine. Oxford University Press. pp. 927–931. ISBN 978-0-19-956874-1. Retrieved 8 August 2024.
- ^ Jayne, David (2009). "The diagnosis of vasculitis". Best Practice & Research Clinical Rheumatology. 23 (3): 445–453. doi:10.1016/j.berh.2009.03.001. PMID 19508950.
- ^ Shavit, Eran; Alavi, Afsaneh; Sibbald, R. Gary (2018). "Vasculitis—What Do We Have to Know? A Review of Literature". The International Journal of Lower Extremity Wounds. 17 (4): 218–226. doi:10.1177/1534734618804982. ISSN 1534-7346. PMID 30501545.
- ^ a b c d e f g h i j k Jennette, J. Charles (27 September 2013). "Overview of the 2012 revised International Chapel Hill Consensus Conference nomenclature of vasculitides". Clinical and Experimental Nephrology. 17 (5). Springer Science and Business Media LLC: 603–606. doi:10.1007/s10157-013-0869-6. ISSN 1342-1751. PMC 4029362. PMID 24072416.
- ^ Johnston, S L; Lock, R J; Gompels, M M (14 March 2024). "Takayasu arteritis: a review". Journal of Clinical Pathology. 55 (7). BMJ Publishing Group: 481–486. doi:10.1136/jcp.55.7.481. PMC 1769710. PMID 12101189.
- ^ Hoffman, Gary S. (1 November 2016). "Giant Cell Arteritis". Annals of Internal Medicine. 165 (9): ITC65–ITC80. doi:10.7326/AITC201611010. ISSN 0003-4819. PMID 27802475.
- ^ Forbess, Lindsy; Bannykh, Serguei (2015). "Polyarteritis Nodosa". Rheumatic Disease Clinics of North America. 41 (1): 33–46. doi:10.1016/j.rdc.2014.09.005. PMID 25399938.
- ^ Son, M. B. F.; Newburger, J. W. (1 April 2013). "Kawasaki Disease". Pediatrics in Review. 34 (4): 151–162. doi:10.1542/pir.34-4-151. ISSN 0191-9601. PMID 23547061.
- ^ Hedrich, Christian M.; Schnabel, Anja; Hospach, Toni (10 July 2018). "Kawasaki Disease". Frontiers in Pediatrics. 6: 198. doi:10.3389/fped.2018.00198. ISSN 2296-2360. PMC 6048561. PMID 30042935.
- ^ Chung, Sharon A.; Seo, Philip (2010). "Microscopic Polyangiitis". Rheumatic Disease Clinics of North America. 36 (3): 545–558. doi:10.1016/j.rdc.2010.04.003. PMC 2917831. PMID 20688249.
- ^ Comarmond, Cloé; Cacoub, Patrice (2014). "Granulomatosis with polyangiitis (Wegener): Clinical aspects and treatment". Autoimmunity Reviews. 13 (11): 1121–1125. doi:10.1016/j.autrev.2014.08.017. PMID 25149391.
- ^ Grygiel-Górniak, Bogna; Limphaibool, Nattakarn; Perkowska, Katarzyna; Puszczewicz, Mariusz (3 October 2018). "Clinical manifestations of granulomatosis with polyangiitis: key considerations and major features". Postgraduate Medicine. 130 (7): 581–596. doi:10.1080/00325481.2018.1503920. ISSN 0032-5481. PMID 30071173.
- ^ Vaglio, A.; Buzio, C.; Zwerina, J. (2013). "Eosinophilic granulomatosis with polyangiitis (Churg–Strauss): state of the art". Allergy. 68 (3): 261–273. doi:10.1111/all.12088. ISSN 0105-4538. PMID 23330816.
- ^ White, Jpe; Dubey, S. (2023). "Eosinophilic granulomatosis with polyangiitis: A review". Autoimmunity Reviews. 22 (1): 103219. doi:10.1016/j.autrev.2022.103219. PMID 36283646.
- ^ Bharati, Joyita; Jhaveri, Kenar D.; Salama, Alan D.; Oni, Louise (2024). "Anti–Glomerular Basement Membrane Disease: Recent Updates". Advances in Kidney Disease and Health. 31 (3): 206–215. doi:10.1053/j.akdh.2024.04.007. PMID 39004460.
- ^ Silva, Filipa; Pinto, Claudemira; Barbosa, Arsénio; Borges, Tiago; Dias, Carlos; Almeida, Jorge (2019). "New insights in cryoglobulinemic vasculitis". Journal of Autoimmunity. 105: 102313. doi:10.1016/j.jaut.2019.102313. PMID 31383568.
- ^ Pillebout, Evangéline; Sunderkötter, Cord (2021). "IgA vasculitis". Seminars in Immunopathology. 43 (5): 729–738. doi:10.1007/s00281-021-00874-9. ISSN 1863-2297. PMID 34170395.
- ^ Gu, Stephanie L.; Jorizzo, Joseph L. (2021). "Urticarial vasculitis". International Journal of Women's Dermatology. 7 (3): 290–297. doi:10.1016/j.ijwd.2021.01.021. PMC 8243153. PMID 34222586.
- ^ Bettiol, Alessandra; Prisco, Domenico; Emmi, Giacomo (1 May 2020). "Behçet: the syndrome". Rheumatology. 59 (Supplement_3): iii101–iii107. doi:10.1093/rheumatology/kez626. ISSN 1462-0324. PMID 32348523.
- ^ Iliescu, Daniela Adriana; Timaru, Cristina Mihaela; Batras, Mehdi; Simone, Algerino De; Stefan, Cornel (14 March 2024). "COGAN'S SYNDROME". Romanian Journal of Ophthalmology. 59 (1). Romanian Society of Ophthalmology: 6–13. PMC 5729811. PMID 27373108.
- ^ Martins-Martinho, Joana; Dourado, Eduardo; Khmelinskii, Nikita; Espinosa, Pablo; Ponte, Cristina (2021). "Localized Forms of Vasculitis". Current Rheumatology Reports. 23 (7): 49. doi:10.1007/s11926-021-01012-y. ISSN 1523-3774. PMC 8247627. PMID 34196889.
- ^ Russell, James P.; Gibson, Lawrence E. (2006). "Primary cutaneous small vessel vasculitis: approach to diagnosis and treatment". International Journal of Dermatology. 45 (1): 3–13. doi:10.1111/j.1365-4632.2005.02898.x. ISSN 0011-9059. PMID 16426368.
- ^ Furukawa, Fukumi (2012). "Cutaneous Polyarteritis Nodosa: An Update". Annals of Vascular Diseases. 5 (3). Editorial Committee of Annals of Vascular Diseases: 282–288. doi:10.3400/avd.ra.12.00061. PMC 3595843. PMID 23555526.
- ^ Junek, Mats; Perera, Kanjana S; Kiczek, Matthew; Hajj-Ali, Rula A (26 August 2023). "Current and future advances in practice: a practical approach to the diagnosis and management of primary central nervous system vasculitis". Rheumatology Advances in Practice. 7 (3): rkad080. doi:10.1093/rap/rkad080. ISSN 2514-1775. PMC 10712448. PMID 38091383.
- ^ Abu El-Asrar, Ahmed M.; Herbort, Carl P.; Tabbara, Khalid F. (2005). "Retinal Vasculitis". Ocular Immunology and Inflammation. 13 (6): 415–433. doi:10.1080/09273940591003828. ISSN 0927-3948. PMID 16321886.
- ^ Leone, Patrizia; Prete, Marcella; Malerba, Eleonora; Bray, Antonella; Susca, Nicola; Ingravallo, Giuseppe; Racanelli, Vito (5 November 2021). "Lupus Vasculitis: An Overview". Biomedicines. 9 (11). MDPI AG: 1626. doi:10.3390/biomedicines9111626. hdl:11572/386878. ISSN 2227-9059. PMC 8615745. PMID 34829857.
- ^ Bartels, Christie M.; Bridges, Alan J. (15 September 2010). "Rheumatoid Vasculitis: Vanishing Menace or Target for New Treatments?". Current Rheumatology Reports. 12 (6). Springer Science and Business Media LLC: 414–419. doi:10.1007/s11926-010-0130-1. ISSN 1523-3774. PMC 2950222. PMID 20842467.
- ^ Seidman, M.A. (2014). "Vasculitis". Pathobiology of Human Disease. Elsevier. pp. 2995–3005. doi:10.1016/b978-0-12-386456-7.05506-4. ISBN 978-0-12-386457-4.
- ^ a b c d e f g h Jennette, J. C.; Falk, R. J.; Bacon, P. A.; Basu, N.; Cid, M. C.; Ferrario, F.; Flores-Suarez, L. F.; Gross, W. L.; Guillevin, L.; Hagen, E. C.; Hoffman, G. S.; Jayne, D. R.; Kallenberg, C. G. M.; Lamprecht, P.; Langford, C. A.; Luqmani, R. A.; Mahr, A. D.; Matteson, E. L.; Merkel, P. A.; Ozen, S.; Pusey, C. D.; Rasmussen, N.; Rees, A. J.; Scott, D. G. I.; Specks, U.; Stone, J. H.; Takahashi, K.; Watts, R. A. (27 December 2012). "2012 Revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides". Arthritis & Rheumatism. 65 (1). Wiley: 1–11. doi:10.1002/art.37715. ISSN 0004-3591. PMID 23045170.
- ^ a b Mahr, Alfred; de Menthon, Mathilde (2015). "Classification and classification criteria for vasculitis". Current Opinion in Rheumatology. 27 (1). Ovid Technologies (Wolters Kluwer Health): 1–9. doi:10.1097/bor.0000000000000134. ISSN 1040-8711. PMID 25415531. S2CID 24318541.
- ^ Suresh, E (1 August 2006). "Diagnostic approach to patients with suspected vasculitis". Postgraduate Medical Journal. 82 (970). Oxford University Press (OUP): 483–488. doi:10.1136/pgmj.2005.042648. ISSN 0032-5473. PMC 2585712. PMID 16891436.
- ^ Luqmani, Raashid Ahmed; Pathare, Sanjay; Kwok-fai, Tony Lee (2005). "How to diagnose and treat secondary forms of vasculitis". Best Practice & Research Clinical Rheumatology. 19 (2). Elsevier BV: 321–336. doi:10.1016/j.berh.2004.11.002. ISSN 1521-6942. PMID 15857799.
- ^ a b Eastham, A Brooke W (12 July 2021). "Leukocytoclastic Vasculitis: Practice Essentials, Pathophysiology, Etiology". Medscape Reference. Archived from the original on 19 October 2019. Retrieved 8 November 2019. Updated: 25 October 2018
- ^ "Giant-Cell Arteritis and Polymyalgia Rheumatica". New England Journal of Medicine. 371 (17): 1652–1653. 23 October 2014. doi:10.1056/NEJMc1409206. ISSN 0028-4793.
- ^ Dellavedova, L.; Carletto, M.; Faggioli, P.; Sciascera, A.; Del Sole, A.; Mazzone, A.; Maffioli, L. S. (2016). "The prognostic value of baseline 18F-FDG PET/CT in steroid-naïve large-vessel vasculitis: introduction of volume-based parameters". European Journal of Nuclear Medicine and Molecular Imaging. 43 (2): 340–348. doi:10.1007/s00259-015-3148-9. ISSN 1619-7070. PMID 26250689.
- ^ Burtis, Carl A.; Ashwood, Edward R.; Bruns, David E. (2012). Tietz Textbook of Clinical Chemistry and Molecular Diagnostics. St. Louis, Mo: Saunders. p. 1568. ISBN 978-1-4160-6164-9.
